

Affiliations
ABSTRACT
Chilaiditi sign is a rare radiological finding often discovered incidentally on chest or abdominal x-rays when there is hepato-diaphragmatic interpositioning of small or large intestines. Usually asymptomatic but when accompanied by cardiac, respiratory or abdominal symptoms, it is known as Chilaidati syndrome. Its exact cause is unknown but may involve hepatic, diaphragmatic, respiratory and intestinal factors. While most cases can be managed conservatively, a few cases require surgical intervention. Due to lack of awareness, special care must be taken when diagnosing a patient, because it can mimic pneumoperitoneum and subdiaphragmatic abscess radiologically. The present case is unique as it reports Chilaiditi syndrome in a young female patient, highlighting the importance of keeping a broad differential diagnosis when encountered with a patient presenting with incidental finding of air under diaphragm on x-ray, especially when the clinical symptoms do not correlate with the radiological findings.
Key Words: Chilaiditi syndrome, Pneumoperitoneum, Abdominal pain.
INTRODUCTION
Chilaiditi sign is diagnosed radiologically when pseudopneumoperitoneum is seen in the subdiaphragmatic space due to bowel interposition between liver and right hemidiaphragm.1 It rarely causes any symptoms but the diagnosis of Chilaiditi syndrome is established when patient presents with gastrointestinal symptoms, such as, nausea, vomiting, abdominal pain and/or respiratory distress, and chest pain.2 Worldwide reported incidence of Chilaiditi sign is 0.025-0.28%, occurring more frequently in older men, with a male-to-female ratio of 4:1, and median age at diagnosis of 60 years.3 Owing to the rare nature of this disease, very little is known about its aetiology.
CASE REPORT
A 28-year married female presented to the emergency with nausea, vomiting and altered bowel habits for the last one month, along with constipation, pain in abdomen, and abdominal distention for 5 days. She had generalised, colicky abdominal pain. Past medical and surgical history was unremarkable.
On physical examination, a pale, malnourished patient with temperature of 101˚F, pulse, 98 beats/minute, and blood pressure, 100/70 mm/Hg, was lying in bed and maintaining oxygen saturation on room air. Abdominal distention with diffuse mild tenderness and sluggish bowel sounds were appreciated. Rebound tenderness and guarding were absent. Murphy’s sign was negative. Digital rectal examination (DRE) was unremarkable and nasogastric (NG) tube drain showed 150 ml of fluid. A complete blood count showed anaemia (haemoglobin, 9.1 g/dl) and raised total leucocyte count (TLC) of 12.2×109/L. Metabolic profile showed serum sodium of 130 mEq/L with hypoalbuminaemia (17 g/l), hypocalcaemia (serum calcium: 6.4 mg/dl) and normal serum potassium (3.5 mmol/L). Serum alanine aminotransferase (ALT) was slightly elevated (62 U/L). Urine for pregnancy test was negative and serum beta-hCG was also within the normal limits (<5 IU/L). Serum lipase (55 U/L) and amylase (80 U/L) were also within the normal limits. Ultrasound of the abdomen revealed distended gut loops with pelvic free fluid.
Chest x-ray showed air under right hemi-diaphragm (Figure 1). CT scan was planned but postponed due to some technical issues.
Initial diagnosis of pneumoperitoneum was sought but the clinical picture did not correlate with the x-ray findings. So keeping in view the Chilaiditi syndrome, a plan was made to manage patient conservatively with NG decompression, IV fluids, IV antibiotics, and enemas. Electrolyte imbalance was corrected; patient was transfused packed red blood cells and IV albumin. After 24 hours, the condition of the patient improved, and a plan was made to continue the treatment. Patient was mobilised out of bed, and started on oral sips, and stool/flatus passed after 24 hours. Patient was discharged on oral medication and called for a follow-up after one week.
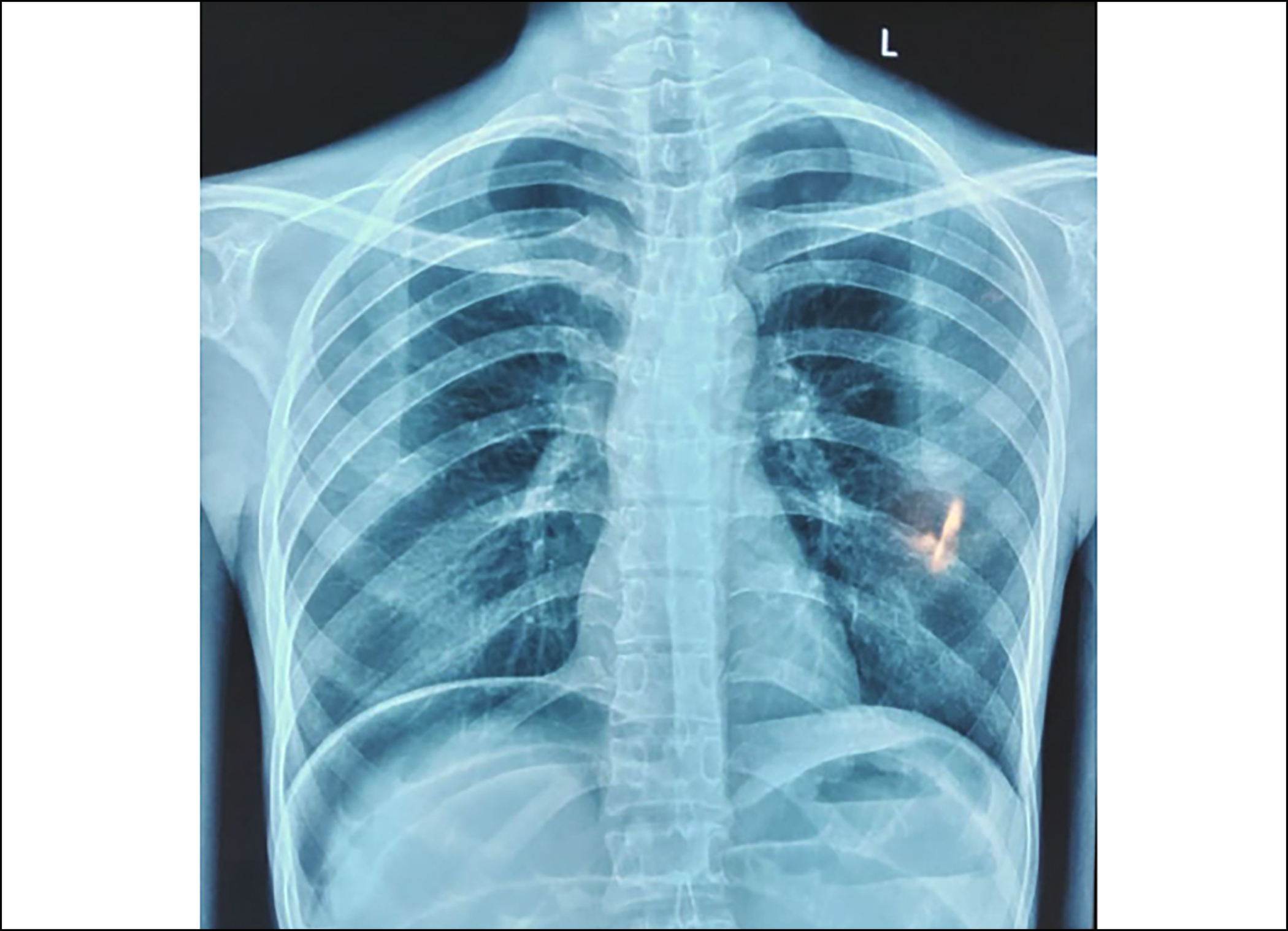 Figure 1: Chest x-ray showing air under the right hemi-diaphragm.
Figure 1: Chest x-ray showing air under the right hemi-diaphragm.
DISCUSSION
Chilaiditi syndrome was first described by a Greek radiologist, Demetrious Chilaiditi in 1911.4 Chilaiditi sign is the result of malposition of the colon between the liver and the diaphragm. The sign can be divided into anterior and posterior types depending upon the segment of bowel interposed between the liver and diaphragm. Usually hepatic flexure, transverse colon or ascending colon is interposed but there have been reports of the involvement of small bowel.5 It could develop as a result of congenital and acquired causes. Congenital anatomical variations like absence, laxity, or elongation of the suspensory ligament of the transverse colon or the falciform ligament may result in the appearance of Chilaiditi sign.4 Acquired causes including conditions which lead to liver atrophy such as cirrhosis or hepatectomy, chronic lung disorders, multiple pregnancies, obesity, diaphragmatic paralysis, and ascites have been associated with the development of Chilaiditi sign.4-6 The diaphragmatic causes that predispose to Chiaiditi sign include right-sided diaphragmatic hemiparesis (phrenic nerve damage) and diaphragmatic eventration.7 Few cases of iatrogenically-induced Chilaiditi syndrome have been described in the literature resulting from bariatric surgery, enteral feeding tube insertion and colonoscopy.5
Clinical presentation may vary significantly, with some patients remaining asymptomatic and diagnosis is made incidentally. The most common presenting symptoms are bloating, nausea, vomiting, abdominal pain and constipation.8 In severe cases, the patients may present with difficulty in breathing and chest pain depending on the underlying cause and extent of colonic involvement. While many patients can live on with mild GI symptoms for decades, the most feared complication is the volvulus or perforation. Rarely perforated subdiaphragmatic appendicitis could occur as a complication of Chilaiditi syndrome. Chilaiditi syndrome should be considered as a rare cause of small or large bowel obstruction. Ogilvie’s syndrome has also been observed in patients with Chilaiditi syndrome. Additionally, there are reports of association of Chilaiditi syndrome with various pulmonary and gastrointestinal malignancies.1,5
Imaging techniques like chest/abdominal x-ray and sonography are used primarily for diagnosis, with CT scan being the diagnostic modality of choice. Three radiographic criteria are used to define Chilaiditi sign; the right hemi-diaphragm must be superiorly displaced to the liver by the intestines, bowel distention by air, and the superior margin of the liver must be depressed below the left hemi-diaphragm.9,10 Distended intestines cause this specific position of the liver. The characteristic radiographic marker is presence of air below right hemi-diaphragm with visible haustral folds or valvulae conniventes, which does not change when the position of the patient is altered.9 Whereas, in case of pneumoperitoneum, a crescent-shaped gas shadow is seen under diaphragm without visible haustral folds, and altering patient position can change the position of the gas. Therefore, it is important to get serial x-rays.4
The differential diagnoses of Chilaiditi syndrome include bowel obstruction, bowel ischaemia, and acute inflammatory conditions like appendicitis, diverticulitis, intussusception, and volvulus.1 Although difficult to establish accurate diagnosis without CT scan, in resource-constrained settings, surgeons could rely on serial x-rays, ultrasound as well as a dissociation of clinical picture from the radiological findings. Treatment is not required for asymptomatic patients with Chilaiditi sign. But for Chilaiditi syndrome, the management approach is usually conservative. It includes bed rest, keeping nil by mouth, placing NG tube, intravenous fluid therapy, laxatives, and enema.10 Surgical intervention is required for patients who present with complications like intestinal obstruction, intestinal ischaemia, volvulus, and perforation.10 Surgical options may be performed using open, laparoscopic or robotic surgery with a variety of procedures such as a resection of the involved part of the colon. Cecopexy or hepatopexy could be done to prevent any recurrence.5,9,11
In conclusion, knowledge of this rare entity is important, especially for the new surgeons, radiologists, and general physicians working alone in peripheral hospitals with limited availability of diagnostic facilities. Pneumoperitoneum is a surgical emergency warranting immediate exploration while Chilaiditi syndrome responds to conservative management. In resource-limited settings, dissociation of clinical picture from radiological findings is very helpful to save such patients from unnecessary surgical exploration.
PATIENT’S CONSENT:
Informed consent was taken from the patient.
COMPETING INTEREST:
The authors declared no conflict of interest.
AUTHORS’ CONTRIBUTION:
SA: Substantial contribution to conception of work, collection of data from patient, literature review, drafting manuscript and agreement to be accountable for all aspects of the work and approval of the final version.
SM: Analysis of data, critical revision, final approval, agreement to accountability for all aspects of work.
HN: Substantial contribution to the conception of work, literature research, data collection, drafting the manuscript, revising it critically for important intellectual content, and approval of final version to be published, agreement to be accountable for all aspects of work.
TM: Interpretation of data, critical revision, final approval and agreement to be accountable for all aspects of work.
AA: Collection of data from the patient, critical revision, final approval, and agreement to be accountable for all aspects of work.
All authors approved the final version of the manuscript to be published.
REFERENCES